The Explosive Weapons Trauma Care Collective
A Roadmap for Reducing Preventable Death Among Civilian Casualties of Explosive Injury
CISR JournalThis article is brought to you by the Center for International Stabilization and Recovery (CISR) from issue 28.3 of The Journal of Conventional Weapons Destruction available on the JMU Scholarly Commons and Issuu.com.
By Hannah Wild1,2, Aparna Cheran2, Abby Willging2,3, Christelle Loupforest4, Sebastian Kasack5, Tim Gargan6, Barclay Stewart1, International Blast Injury Research Network7, and Adam L. Kushner2,8
- Department of Surgery, University of Washington, Seattle, WA, USA
- Explosive Weapons Trauma Care Collective, International Blast Injury Research Network, University of Southampton, Southampton, UK
- University of Iowa Carver College of Medicine, Iowa City, IA, USA
- Mine Action Area of Responsibility, United Nations Mine Action Service, Geneva, Switzerland
- Mines Advisory Group, Manchester, UK
- The HALO Trust, Wilton, UK
- University of Southampton, Southampton, UK
- Surgeons Overseas, New York, NY, USA
Introduction
In a previous issue of The Journal of Conventional Weapons Destruction, we introduced the rationale underpinning the need for increased emphasis on point-of-injury care as well as enhanced engagement between humanitarian mine action (HMA) and emergency care services for civilian casualties of explosive ordnance (EO).1 The initial working group under which this conceptual foundation was developed was called the Mine Action Trauma Care Collaborative. In the intervening months, that initiative was reconceived as the Explosive Weapons Trauma Care Collective (EXTRACCT) to encompass the broad range of EO and explosive weapons (EW) that inflict harm on civilians in conflict and post-conflict settings.2,3 In this article, we present an overview of EXTRACCT’s approach to reducing preventable death and disability among civilian victims of EO/EW with a focus on low-resource settings (LRS).
Preventable Death Among Civilian Casualties of Explosive Injury
Unfortunately, there is no global or multi-site trauma registry for civilian casualties in conflict settings that can be queried to obtain accurate insight into the precise causes and quantitative burden of preventable death.4 However, estimates from the limited available data demonstrate that an unacceptable proportion of civilian EO/EW casualties are dying of preventable causes (e.g., lack of timely hemorrhage control, loss of airway, under-resuscitation, sepsis). The 2023 Landmine and Cluster Munition Monitor reported an approximately 35 percent case fatality rate (CFR) among civilian EO casualties.5 A separate epidemiologic analysis of global civilian EO casualties pooling a wide range of independent data sources found a nearly 40 percent CFR.6 In contrast, even severely blast-injured patients in high-resource civilian trauma centers and military treatment facilities have significantly lower mortality rates ranging from 2 percent to 8 percent.7,8,9,10 A significant proportion of deaths among civilian EO casualties can therefore be assumed to occur due to causes that could be prevented through improvements in trauma care systems.
As the resource constraints in EO/EW-affected conflict and post-conflict settings are vastly different than those that exist within high-resource civilian trauma centers and military treatment facilities, an equivalent reduction in preventable death is unlikely to be feasible. However, previous work has demonstrated that even in resource-constrained civilian settings, preventable death from explosive injury can be dramatically reduced. Specifically, the Tromsø Mine Victim Center trained layperson first responders (LFR) and prehospital personnel (e.g., paramedics, ambulance providers) in landmine-contaminated regions of Iraq and Cambodia, achieving a reduction in EO/EW-related mortality from 40 percent to 15 percent.11 To increase survival among affected populations, renewed attention must be devoted to improving emergency care systems close to the point of injury.
To increase survival among affected populations, renewed attention must be devoted to improving emergency care systems close to the point of injury.
Approaches to Reducing Preventable Death in a Military Environment
Over the course of the wars in Iraq and Afghanistan, a series of trauma care advances were implemented that compositely reduced combat casualty mortality by 44 percent.12,13 Many of these interventions were predicated on a well-resourced military trauma system with aeromedical evacuation capabilities and intact echelons of damage control and definitive surgical care that are not currently available in most low-resource civilian environments. Nonetheless, certain elements of the overall approach to eliminating preventable death can be translated to the context of civilian EO/EW casualties. EXTRACCT’s approach is informed by the development of the mature Joint Trauma System (JTS) while on a pragmatic and operational level considering the substantial adaptations that must be made in low-resource civilian environments.14 Key differences include: a) numerous stakeholders across sectors engaged in health, protection, and local communities; b) lack of comprehensive casualty data available to identify areas for targeted intervention as well as to benchmark facility-based or system-wide quality improvement initiatives; and c) a broad range of resource constraints.
Clinical Performance Improvement
Clinical Process Guidelines (CPGs) are a pillar of the JTS and provide guidance to clinicians providing emergency and trauma care in the deployed environment. CPGs serve numerous functions including: a) standardization of care and contextual alignment to evidence-based medicine; b) improvement in clinical performance; and c) benchmarking of intervention impact. Care of civilian casualties in EO/EW affected settings frequently occurs in environments with limited resource availability (e.g., equipment/materials, subspecialist expertise, critical care capabilities, organized modes of patient transport) and lack of options for evacuation to higher echelons of care. Therefore, the JTS CPGs are not directly applicable but serve as a positive example for strengthening health systems if adapted to local contexts and resource availability.
EXTRACCT is developing a library of CPGs relevant to the care of civilian victims of blast injury adapted to the available material and human resources common in LRS. These guidelines are being developed with an expert review panel and contain background literature synthesis, guidance on patient assessment and treatment, and links to open-access instructional materials on relevant procedures. The intended target audience includes surgeons, medical doctors, clinical officers, and prehospital personnel working in LRS affected by EO/EW who may be required to care for blast injuries outside of their clinical comfort zone. Given the broad variance in resource availability between settings affected by EO/EW, EXTRACCT CPGs will be formatted with matrices providing tiered guidance on various aspects of management stratified based on available infrastructure and human/material resources.
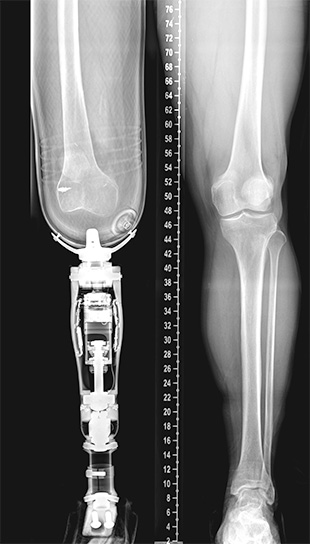
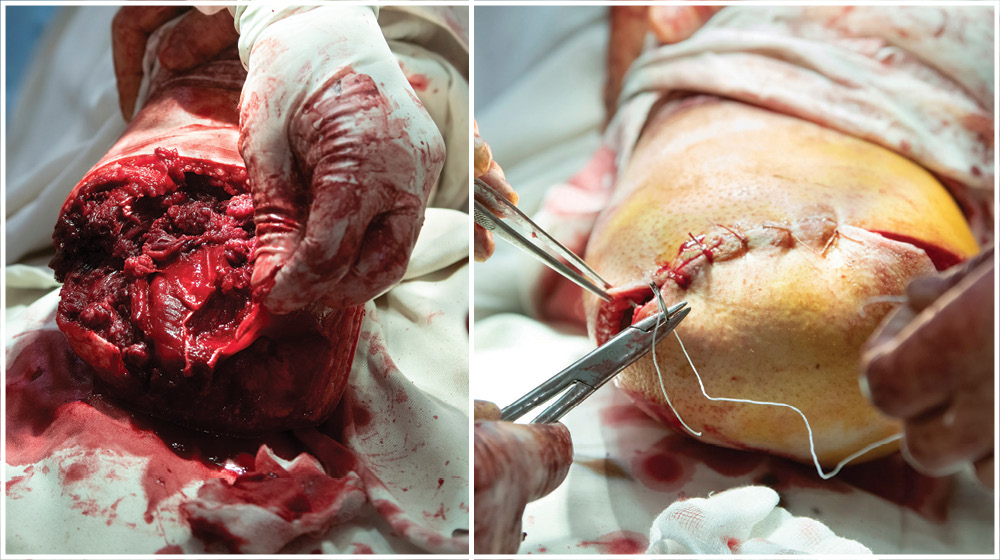
The core EXTRACCT CPG topics are derived from the JTS CPGs that hold relevance to the management of blast injury in LRS, such as mangled extremity (e.g., compartment syndrome, crush syndrome, extremity fracture, traumatic amputation), thermal injury/burns associated with blast mechanisms, and specific complications (e.g., blast traumatic brain injury, blast lung). EXTRACCT welcomes proposals for new CPG topics from engaged stakeholders, particularly medical personnel providing care to EO/EW victims in LRS. Further details about the full list of planned CPGs, how to submit topic requests, and EXTRACCT’s process guidelines are available through the International Blast Injury Research Network (IBRN).15
Surgical Consultants
Military trauma systems use teleconsultation as a means of providing remote support to medical providers confronted with the management of complex injuries in deployed environments where subspecialty expertise may be unavailable.16 In civilian settings, teleconsultation has been used for a range of purposes to address gaps in access to subspecialty care even across large geographic regions.17,18 Relatively little attention has been given, however, to the special considerations around implementation of teleconsultation in LRS affected by conflict.19 In numerous contemporary conflicts such as those in Gaza, Ukraine, Myanmar, and Syria, informal grassroots communication networks have arisen to provide remote support to local healthcare personnel.20 The need that such networks address is clear, as healthcare personnel with a wide range of training and capabilities face an overwhelming volume of complex casualties. However, the telecommunications platforms used, inconsistent security provisions, and lack of centralized security vetting protocols associated with such informal networks incur a potential risk in conflict settings. WhatsApp is an international messaging platform that is now being used in the setting of teleconsultation networks for care of the war-wounded.21,22 Unfortunately, numerous security vulnerabilities exist surrounding the use of this platform including monitoring of metadata, routine shutdowns in insecure environments, and more recently, reported surveillance to identify militants and target strikes based on activity patterns.23,24
Relatively little attention has been given, however, to the special considerations around implementation of teleconsultation in LRS affected by conflict.
Surgical teleconsultation holds potential to increase access to higher-quality trauma care in LRS affected by EO/EW, yet teleconsultation in insecure environments is associated with a different set of ethical challenges than in LRS generally. The security of all involved parties including patients, local healthcare personnel, and remote consultants must be ensured. To address this gap and establish protocols for quality assurance, EXTRACCT will collaborate with informatics experts to conduct a pilot of high-quality, secure surgical teleconsultation in EO/EW-affected LRS.
Three priority areas for quality improvement have been identified. First, identification of an optimal communication platform should be conducted via assessment of strength and vulnerability profiles of existing technologies, understanding the need to balance the competing requirements of adequate security protections with low bandwidth needs. If unable to identify an existing option that satisfactorily meets both, collaboration with informatics stakeholders will be pursued to develop alternatives. Second, clear processes for consultant vetting and member entry, including strict evaluation of consultant credentials, terms of reference for engagement, and standardized consultation format for providers in the field are required. Third, activities conducted through surgical teleconsultation should be leveraged to provide a dataset on civilian EO/EW victims, associated resource utilization and care processes, and outcomes. These data would contain more granularity regarding injury patterns, procedures rendered, and associated morbidity/mortality than is currently available from existing casualty data collected via the Information Management System for Mine Action (IMSMA) applying IMAS 05.10.25,26 A pilot surgical teleconsultant network will be developed after identifying partner institutions in EO/EW-affected LRS to promote longitudinal capacity-building as opposed to one-off consultations.
Operations
EXTRACCT’s operational activities are organized within the structure of the Civilian Casualty Care Chain (C-CCC), previously presented in this Journal (Figure 1).27 The C-CCC identifies a set of activities from point-of-injury to emergency care at a health facility in which HMA stakeholders can feasibly engage to improve trauma care for EO/EW casualties. Three elements of the C-CCC have been selected for initial pilots and programmatic development:
LFR training. Improving care close to the point-of-injury is a key opportunity to reduce preventable death. In many LRS where EO/EW incidents occur, organized prehospital and emergency medical services are limited. Layperson bystanders without formal medical training are often the first responders to casualties in their communities. Numerous LFR trainings have arisen to address the burden of non-violent trauma in LRS.28,29 Fewer LFR trainings have been deployed in EO/EW-affected conflict or post-conflict settings, with the Tromsø Mine Victim Center’s Village University being a notable exception. A core component of the 2023 World Health Assembly adoption of the World Health Organization (WHO) Resolution on Integrated Emergency, Critical, and Operative Care (WHA 76.2) was an increased emphasis on LFR trainings.30 This has taken the form of the WHO’s Community First Aid Responder (CFAR) training. EXTRACCT will be conducting a pilot of joint delivery of a conflict-adapted version of the WHO CFAR curriculum with explosive ordnance risk education (EORE) among communities affected by improvised explosive device threats in Burkina Faso. This pilot (2024–2026) is conducted in collaboration with Mines Advisory Group and local partners, NGO Pull for Progress, and the Department of Public Health at the University of Joseph Ki-Zerbo, Ouagadougou. Results of this pilot may inform efforts to scale combined EORE with LFR trainings as an enhanced form of building community resilience to the threat of explosive violence and increasing survival among EO/EW casualties in LRS.
Trauma care capacity assessment and prehospital notification pathways. A series of key informant interviews with sector experts was undertaken by EXTRACCT to inform the development of the C-CCC.31 Thematic analysis of these interviews identified an opportunity to improve standardization of trauma care capacity evaluations. Specifically, in the current state, most mine action operators reported conducting independent evaluations of health facilities in countries where they are operational. These assessments are conducted in a non-standardized manner and without formal integration either with local health authorities or with other HMA stakeholders. In 2014, the International Assessment of Capacity for Trauma (INTACT) was developed as an index for trauma care capacity assessment in LRS.32 EXTRACCT is collaborating with the creators of INTACT to revise this tool for use by HMA stakeholders as INTACT-Blast Injury (BI). We will subsequently collaborate with HMA partners to pilot this approach to trauma care capacity assessment in an EO/EW-affected setting. Such standardization holds potential to improve the quality of evaluation, decrease redundancy and resource utilization in duplicative evaluation processes, and increase engagement with local and multilateral health stakeholders (e.g., local healthcare personnel, ministries of health, WHO). Once an in-country trauma care capacity evaluations utilizing INTACT-BI has been completed, this information can be used to generate resources such as referral and casualty routing pathways as well as the development of a prehospital notification system (i.e., a standardized communication mechanism by which receiving facilities are notified of incoming casualties). In high-resource settings, prehospital notification systems have been associated with significant reduction in trauma-related mortality.33 Implementation of similar systems in EO/EW-affected LRS can improve facility preparedness to manage blast-injured patients, and can be conducted with a range of communications strategies including mobile phones and radio.34
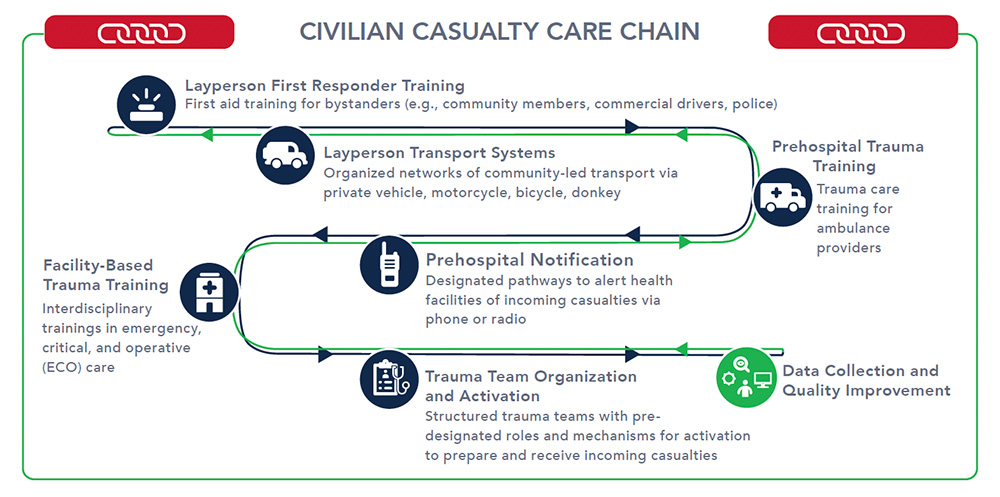
Blast trauma clinical training curriculum. In response to a need from health personnel providing trauma care during conflict in Myanmar, a collaborative virtual trauma education curriculum, the Global Trauma Collaboration (GTC), was developed by Baylor College of Medicine Center for Global Surgery.35 The GTC covers a wide range of topics related to conflict-related trauma (e.g., damage control resuscitation, vascular trauma, chemical weapons, and post-traumatic stress disorder). EXTRACCT and the Pediatric Blast Injury Partnership (PBIP) will collaborate with the GTC to develop a focused set of blast injury modules to expand the core trauma didactics.36 Like EXTRACCT’s CPGs, these modules will be linked to open-access training materials on relevant procedures (e.g., external fixator application for management of extremity trauma; escharotomy for burns).
Research with Operational Relevance
EXTRACCT maintains a broad research portfolio around topics on injury prevention and trauma care for civilian EO/EW casualties with clear operational relevance. Requests for topics of inquiry that have come from humanitarian practitioners based on needs identified in the field or policy gaps are also prioritized. Current EXTRACCT projects are not reviewed exhaustively here, but selected representative examples follow:
Incendiary weapons (IW). IW have been selected as a priority area of research due to a) the disproportionate suffering inflicted through concomitant blast and thermal injuries associated with this weapon type as well as b) the clear policy relevance related to gaps in Protocol III of the Convention on Certain Conventional Weapons that limit its capacity to protect civilians from harm from incendiary weapons.37,38 Current work in this area is conducted under EXTRACCT’s role as Chair of the Incendiary Weapons Sub-Committee of the EORE Advisory Group Emergency Risk Education Task Teams.39
Sheltering guidance for civilians during explosive threats. In response to a request from HMA stakeholders, EXTRACCT is addressing an evidence gap surrounding guidance provided to civilians exposed to explosive threats, particularly the use of explosive weapons in populated areas. In the current state, recommendations being provided to civilians in this context are neither a) standardized across organizations nor b) based on empiric data. EXTRACCT is conducting a systematic review of the literature around sheltering guidance during explosive events in conflict as well as qualitative analysis of key informant interviews with sector experts to provide a current understanding of existing recommendations and the manner in which they were derived. These studies will provide the evidence base to conduct future multidisciplinary work combining blast engineering with public health and clinical trauma care to generate empirically based injury prevention strategies for civilians exposed to risk of explosive injury in conflict.
EXTRACCT’s ongoing research encompasses many additional domains including: a) blast injury epidemiology (specifically, generating estimates of the global burden of blast injury by injury pattern [e.g., traumatic brain injury, orthopedics, burns, genitourinary] as well as pilot quantification of preventable death among civilian EO/EW casualties); b) management of embedded ordnance; c) post-exposure prophylaxis for infectious disease following blast injury in a range of endemic settings; d) best practice guidance on evaluation strategies in trauma care training courses in LRS; d) review of low-cost surgical simulation models to assess gaps for innovation; e) appropriate adaptation of guidance on tourniquet application in LRS; and f) the intersection of mine action and food security with implications for caloric requirements associated with complex polytrauma.
Conclusion
System-wide efforts to improve trauma care in low-resource settings affected by EO/EW face significant challenges in comparison to high-resource civilian and military trauma systems. Such challenges include the lack of a shared trauma registry to provide comprehensive casualty data, significant constraints in human and material resources, and limited organized prehospital transport. Despite these constraints, many steps can and must be taken to improve trauma care and increase survivability for civilian casualties of EO/EW. EXTRACCT is engaging a broad range of partners in humanitarian health and protection in a coordinated approach to meet this need through activities spanning clinical performance improvement, research, operations, and evidence-based advocacy.
See endnotes below.
 Hannah Wild, MD, is a General Surgery Resident at the University of Washington focused on improving humanitarian surgical care for civilian casualties in conflict settings, particularly victims of explosive injury. She received her undergraduate degree from Harvard University and MD from Stanford University. In collaboration with the International Blast Injury Research Network (IBRN) and United Nations Mine Action Service (UNMAS), she leads the Explosive Weapons Trauma Care Collective (EXTRACCT), an effort to strengthen coordination between the mine action sector and trauma care for casualties of explosive weapons.
Hannah Wild, MD, is a General Surgery Resident at the University of Washington focused on improving humanitarian surgical care for civilian casualties in conflict settings, particularly victims of explosive injury. She received her undergraduate degree from Harvard University and MD from Stanford University. In collaboration with the International Blast Injury Research Network (IBRN) and United Nations Mine Action Service (UNMAS), she leads the Explosive Weapons Trauma Care Collective (EXTRACCT), an effort to strengthen coordination between the mine action sector and trauma care for casualties of explosive weapons.
 Aparna Cheran is the Program Coordinator for EXTRACCT. In this role, she facilitates research initiatives aimed at mitigating the devastating effects of explosive weaponry and the consequences of conflict. She is a recent graduate of George Mason University’s Master’s of Health Administration program and a former student at Virginia Polytechnic Institute and State University, where she earned two bachelor’s degrees in Microbiology and Religion & Culture.
Aparna Cheran is the Program Coordinator for EXTRACCT. In this role, she facilitates research initiatives aimed at mitigating the devastating effects of explosive weaponry and the consequences of conflict. She is a recent graduate of George Mason University’s Master’s of Health Administration program and a former student at Virginia Polytechnic Institute and State University, where she earned two bachelor’s degrees in Microbiology and Religion & Culture.
 Abby Willging is a fourth year medical student at the University of Iowa Carver College of Medicine. She graduated with high distinction from the University of Iowa in 2021. A recipient of the Gold Foundation’s Summer Research Fellowship, she has completed global rotations in Riobamba, Ecuador, and Moshi, Tanzania. She joined the EXTRACCT team in early 2024 and is honored to take part in such impactful and humanistic work. Her contributions focus on developing Layperson First Responder curriculum and secure surgical tele-consultation within low-resource conflict zones.
Abby Willging is a fourth year medical student at the University of Iowa Carver College of Medicine. She graduated with high distinction from the University of Iowa in 2021. A recipient of the Gold Foundation’s Summer Research Fellowship, she has completed global rotations in Riobamba, Ecuador, and Moshi, Tanzania. She joined the EXTRACCT team in early 2024 and is honored to take part in such impactful and humanistic work. Her contributions focus on developing Layperson First Responder curriculum and secure surgical tele-consultation within low-resource conflict zones.
 Christelle Loupforest is the Officer-in-Charge of the UNMAS Office in Geneva. In her twenty-five years of service with the United Nations, she served in the Department of Peace Operations, the Office for the Coordination of Humanitarian Affairs, the United Nations/Organization of American States Human Rights Mission in Haiti, and at the World Health Organization. She holds a Master of Political Science and speaks English, French, and Spanish.
Christelle Loupforest is the Officer-in-Charge of the UNMAS Office in Geneva. In her twenty-five years of service with the United Nations, she served in the Department of Peace Operations, the Office for the Coordination of Humanitarian Affairs, the United Nations/Organization of American States Human Rights Mission in Haiti, and at the World Health Organization. She holds a Master of Political Science and speaks English, French, and Spanish.
 Sebastian Kasack holds a master’s degree in geography and has been involved in mine action since 1996, working for international nongovernmental organizations, UNMAS, United Nations Childrens Fund (UNICEF), and United Nations Development Programme. In 2016, he joined Mines Advisory Group as a Senior Technical Advisor. On victim assistance, he authored the UNICEF publication, “Assistance to Victims of Landmines and Explosive Remnants of War Guidance on child-focused victim assistance.”
Sebastian Kasack holds a master’s degree in geography and has been involved in mine action since 1996, working for international nongovernmental organizations, UNMAS, United Nations Childrens Fund (UNICEF), and United Nations Development Programme. In 2016, he joined Mines Advisory Group as a Senior Technical Advisor. On victim assistance, he authored the UNICEF publication, “Assistance to Victims of Landmines and Explosive Remnants of War Guidance on child-focused victim assistance.”
 Tim Gargan is the Head of Medical for The HALO Trust (HALO) and has worked in humanitarian mine action (HMA) since 2013. He is also a UK registered Paramedic with several years of experience in the UK National Health Service and now works for HALO coordinating and managing medical matters across all their programs globally.
Tim Gargan is the Head of Medical for The HALO Trust (HALO) and has worked in humanitarian mine action (HMA) since 2013. He is also a UK registered Paramedic with several years of experience in the UK National Health Service and now works for HALO coordinating and managing medical matters across all their programs globally.
 Barclay Stewart, MD, PhD, is a trauma and burn surgeon at the University of Washington. His research foci include global injury prevention/control, developing models of care for the injured feasible in low-resource settings, and benchmarking quality of care using long-term patient-reported outcomes.
Barclay Stewart, MD, PhD, is a trauma and burn surgeon at the University of Washington. His research foci include global injury prevention/control, developing models of care for the injured feasible in low-resource settings, and benchmarking quality of care using long-term patient-reported outcomes.
The International Blast Injury Research Network (IBRN) is a trans-disciplinary network launched by the University of Southampton after identifying that leading blast research was primarily focused on military rather than civilian situations and perspectives. Addressing this gap, the multidisciplinary IBRN team was founded to improve research within the civilian context and at a holistic level. The IBRN fosters collaboration among a range of stakeholders including academics, clinicians, and humanitarian organizations to facilitate a broad portfolio of multidisciplinary research into the humanitarian consequences of blast injury.
 Adam L. Kushner, MD, MPH, FACS, has worked as a surgeon, educator, and researcher in dozens of countries. He was a founder of Surgeons OverSeas and a subject matter expert on human rights, humanitarian assistance, and disaster relief for the US military. He completed his general surgery residency at the University of Texas Health Science Center-San Antonio; MD at the Mount Sinai School of Medicine; MPH at Johns Hopkins School of Public Health; and BA in History and International Relations at Cornell University. He currently resides in Anchorage, Alaska, where he spends his summers fishing for salmon.
Adam L. Kushner, MD, MPH, FACS, has worked as a surgeon, educator, and researcher in dozens of countries. He was a founder of Surgeons OverSeas and a subject matter expert on human rights, humanitarian assistance, and disaster relief for the US military. He completed his general surgery residency at the University of Texas Health Science Center-San Antonio; MD at the Mount Sinai School of Medicine; MPH at Johns Hopkins School of Public Health; and BA in History and International Relations at Cornell University. He currently resides in Anchorage, Alaska, where he spends his summers fishing for salmon.

